In this article 
View / Download
pdf version of this article
Key Contributor: Dr Lisa Houghton, Lecturer, Department of Human Nutrition, University of Otago
| Key concepts: |
Health professionals can improve pregnancy outcomes by advising women to:
- Achieve a healthy body weight prior to conception and maintain appropriate weight gain during pregnancy according
to pre-pregnancy BMI
- Take a daily supplement of 800 mcg of folic acid beginning before becoming pregnant and continuing throughout the
duration of pregnancy (400 mcg folic acid is adequate but funded tablets are available in 800 mcg or 5 mg strengths)
- Take a low dose iron supplement in their second and third trimester
- Use iodised salt when cooking and at the table, and to choose foods that are sources of iodine e.g. low-fat milk,
eggs
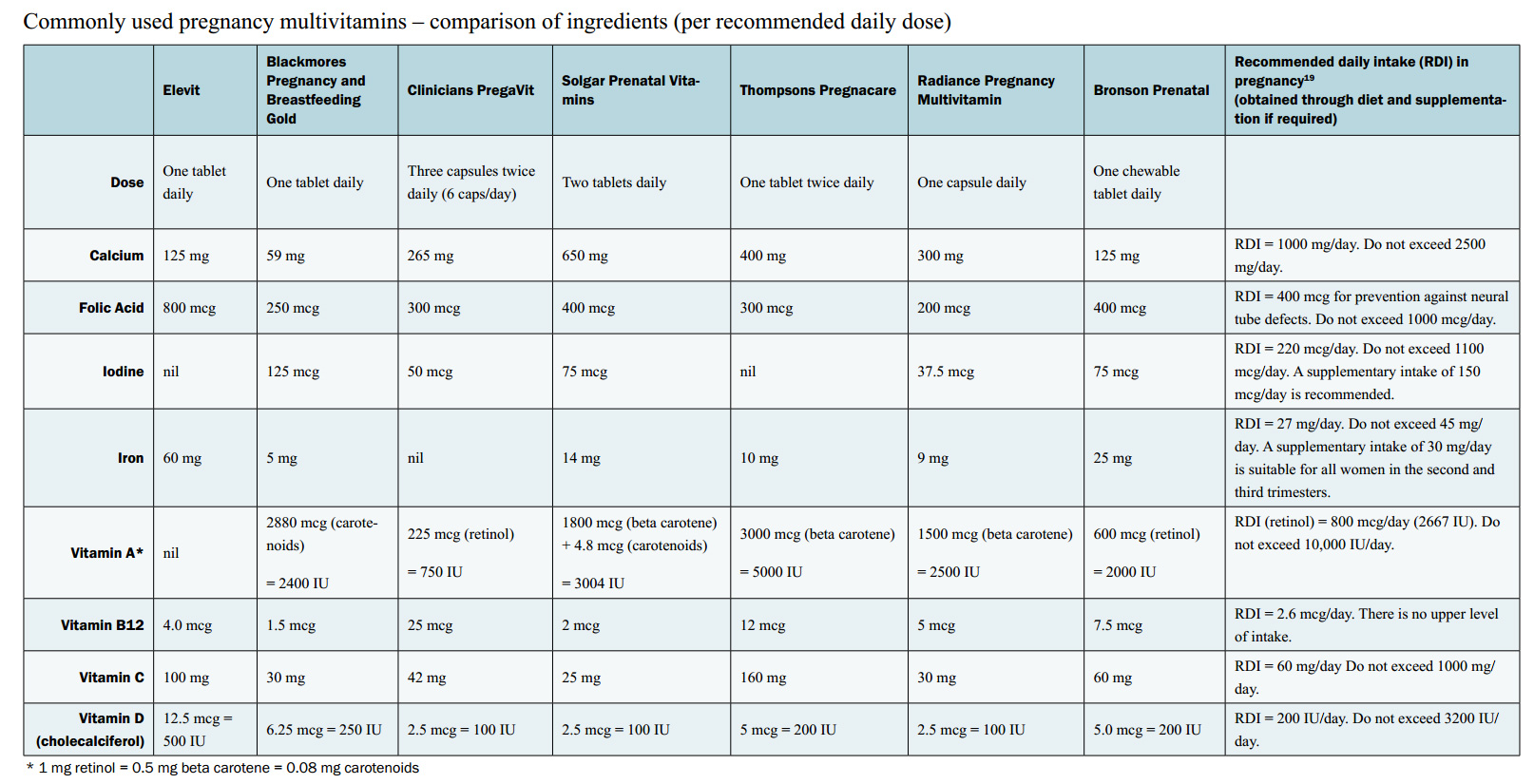
- If consuming a multivitamin and mineral supplement during pregnancy, choose a supplement containing folic acid,
iron, and potassium iodide and be careful not to take excess vitamin A.
|
IN BPJ 15 (AUGUST 2008), we covered the topic of vitamin
and mineral deficiencies. GPs tell us that they would like more information on what supplements or additional foods
they should be prescribing or recommending for women who wish to become pregnant or those who are pregnant.
The importance of ensuring good maternal health during pregnancy is widely recognised while an increasing body of evidence
suggests that nutritional status prior to pregnancy strongly influences foetal and infant outcomes. In view of this, the
goal is to ensure that women attain good nutritional status before, during and between pregnancies to optimise their own
health and reduce the risk of pregnancy complications, birth defects and the onset of chronic diseases in their children.
Attention to pre-conception nutrition improves pregnancy
outcomes
Improving nutritional status before pregnancy is challenging because about half of pregnancies in New Zealand are not
planned.1,2 Even among women planning pregnancy, few seek medical or nutritional advice prior to conception,
and most women do not have their first prenatal care visit until well into the first trimester.
Folate reduces risk of neural tube defects
It is well established that folate decreases the risk for neural tube defects. Women planning a pregnancy, or who are
in the early stages of pregnancy, are advised to take a daily folic acid supplement of 800 mcg for at least four weeks
before, and up to 12 weeks after conception (although women are recommended to continue with this supplement throughout
pregnancy). Higher doses (5 mg daily) are recommended for those who have had a previous neural tube defect affected pregnancy,
a family history of neural tube defects, or are taking anticonvulsant drugs. Supplementing with 400 mcg of folic acid
is sufficient to reduce the risk for women who have no history of neural tube defects, however only 800 mcg or 5 mg tablets
are currently available as registered medicines in New Zealand. Mandatory folic acid fortification of bread next year
will ensure that all women who become pregnant � planned or unplanned � will receive some preconceptional folic acid.
Sub-optimal iron stores are difficult to replenish once pregnant
A substantial amount of iron is required during pregnancy to meet foetal and maternal needs. About 40% of women aged
15�44 years in New Zealand have an inadequate intake of iron. Adequate pre-pregnancy iron stores may play a role in reducing
risk for iron deficiency and anaemia during pregnancy. Sub-optimal iron stores are difficult to replenish once pregnant.
Healthy pre-conception bodyweight improves outcomes
Being underweight or overweight prior to conception can affect birth outcome. Evidence from observational studies suggests
that low pre-pregnancy body mass index (BMI, <20 kg/m2) is associated with reduced infant birth weight, and increased
incidence of preterm delivery.3 Obese women have an elevated risk for pre-eclampsia, gestational diabetes,
neural tube defects and stillbirth, as well as giving birth to a large for gestational age infant.3,4 More
than one quarter of all New Zealand women are obese.4
Weight gain during pregnancy influences infant birth weight and health
The U.S. Institute of Medicine recommendations for appropriate weight gain during pregnancy (Table 1) are based on pre-pregnancy
BMI and uphold a slightly different range of weight gain for each BMI category. Weight gains within these guidelines are
associated with optimal birth weight (between 3000 g and 4000 g) and best labour and delivery outcomes. Women who gain
more weight in pregnancy than recommended have a significantly increased risk of having an infant weighing greater than
4000 g.5 High birthweight infants tend to be taller and heavier children with increased risk of obesity and
metabolic problems in later life.6 Excessive prenatal weight gain also places the mother at risk for long-term
obesity post-delivery.7
Table 1: Current recommendations for weight gain during pregnancy6
| Pre-pregnancy BMI category |
Recommended total gain (kg) |
| Low (<20) |
12.5 � 18.0 |
| Normal (20 � 25) |
11.5 � 16.0 |
| High (>25 � 29) |
7.0 � 11.5 |
| Obese (>29) |
?7.0 |
There are currently no data available to indicate how much weight New Zealand women are gaining during pregnancy. Survey
work conducted in the United States and Europe indicates that only a small proportion of women gain within the recommended
ranges with excessive weight gain being more prevalent than inadequate weight gain.5 Reports indicate that
pregnancy weight gain is influenced by recommendations of health care providers so it is important this advice is accurate.
Many women receive no prenatal weight gain advice.8,9
A healthy diet meets most nutrient requirements during pregnancy
Many questions remain unanswered regarding how the mother�s nutritional status influences pregnancy outcome. Consequences
of deficient or excessive nutrient intakes are difficult to determine, and assessment of vitamin and mineral status during
pregnancy is not easy due to a lack of pregnancy-specific laboratory values. Based on available evidence, a healthy and
varied diet can provide adequate energy and meet the mother�s requirements for most nutrients. Selected vitamin and minerals
that are likely to be limited in the diets of pregnant women are briefly highlighted.
Folate requirements are high during pregnancy
In addition to reducing neural tube defects, lack of folate during pregnancy is associated with increased risk of preterm
delivery, low birth weight and poor foetal growth. The recommended intake of dietary folate is 600 mcg per day. Survey
data of pregnant women in New Zealand indicate that dietary intakes of folate are well below recommended levels.4
400 mcg folic acid or 600 mcg dietary folate?
The 400 mcg recommendation to reduce neural tube defects is based on folic acid (synthetic form of folate) only. The
600 mcg recommended during pregnancy is in the units of Dietary Folate Equivalents (DFE) (food folate = 1 mcg DFE and
folic acid = 1.7 mcg DFE). So essentially the 400 mcg folic acid tablet recommended preconceptional is worth 680 mcg DFEs
and pregnant women then meet both recommendations by taking a supplement. Post-closure of the neural tube (after the first
trimester) it is recommended that women intake 600 mcg DFEs. It is possible to obtain this all from the diet but this
would involve large amounts of foods such as broccoli and spinach. Therefore women are recommended to continue with a
folic acid supplement in addition to a folate rich diet for the entire pregnancy. This recommendation stands regardless
of fortification of the food supply.
Iron requirements increase throughout pregnancy
Additional iron requirements during pregnancy increase substantially from the first trimester to the third trimester.
A recommended dietary intake of 27 mg per day for the entire duration of pregnancy builds iron stores in early pregnancy
for the third trimester.
Although women should be encouraged to consume plenty of iron rich foods during pregnancy, obtaining the recommended
intake from diet alone is difficult. Survey data of pregnant women in New Zealand indicate mean iron intakes between 11�14
mg per day.4 The highest prevalence of low iron stores, iron deficiency and iron-deficiency anaemia is among
New Zealand Māori women, particularly aged 15�24 years.4 Maternal anaemia is associated with infant mortality
and premature delivery.
Post-delivery, a woman who has been iron deficient during pregnancy should have further follow-up as postpartum anaemia
is associated with emotional instability, depression and stress.10
For those who consume no or small amounts of animal source food, or when low iron stores are suspected, a low-dose iron
supplement (30 mg ferrous iron per day) taken at bedtime or between meals is advised. When iron deficiency with or without
anaemia is diagnosed, larger doses of iron supplements (~100 mg ferrous iron per day) may be advised to improve iron status
as early in pregnancy as possible.6 Although there is currently insufficient evidence to recommend for (or
against) routine iron supplementation of all pregnant women, the U.S. Institute of Medicine, recognises that many women
have suboptimal iron stores and advise daily low-dose iron supplementation (30 mg) to all women in the second and third
trimesters.
Fully funded supplements in pregnancy:
Iron
Ferrous fumarate
Tab 200 mg � Ferro-tab
Approximate elemental iron = 65 mg
Ferrous fumarate with folic acid
Tab 310 mg with folic acid 350 mcg � Ferro-F-Tabs
Approximate elemental iron = 100 mg
Ferrous gluconate with ascorbic acid
Tab 170 mg with ascorbic acid 40 mg � Healtheries Iron with Vitamin C
Approximate elemental iron = 20 mg
N.B: Ferrous sulphate preparations are available but subject to a part charge
Folic acid
Tab 5 mg � Apo-Folic Acid
Tab 0.8 mg � Apo-Folic Acid
Vitamin D
Alfacalcidol
Cap 0.25 mcg; Cap 1 mcg; Oral drops 2 mcg per mL |
Iodine requirements increase in pregnancy
Requirements for iodine increase in pregnancy due to a marked change in thyroid function. Despite the upcoming mandatory
fortification of bread with iodine in 2009, pregnant women will likely have intakes below the recommended level of 220
mcg per day. Median iodine intakes of New Zealand pregnant women are estimated between 60 to 70 mcg per day.11 Iodine
deficiency during pregnancy can negatively affect both maternal and infant thyroid function and cognitive development
of the infant.
Despite lack of clinical data on the effect of iodine supplementation on birth outcomes in mild to moderately deficient
pregnant women,12 several health authorities recommend that pregnant women consume 150 mcg per day of potassium
iodide to prevent deficiency.13, 14 Currently there are no single oral iodine preparations available as registered
medicines in New Zealand. Seaweed and kelp tablets should not be used as the iodine content in these products is extremely
variable and can be toxic.
 Iodine supplements are now funded. For more information, see "Snippets: Iodine supplements Zoledronic acid & Atorvastatin", BPJ 30 (August, 2010).
Iodine supplements are now funded. For more information, see "Snippets: Iodine supplements Zoledronic acid & Atorvastatin", BPJ 30 (August, 2010).
Low vitamin D levels can affect foetal bone
During pregnancy, the lack of vitamin D may adversely affect foetal bone and accumulation of newborn vitamin D stores.15 Vitamin
D increases intestinal absorption of calcium. Rickets is a clinical marker of poor pre- and postnatal bone health caused
by vitamin D deficiency. There have been reports that rickets is re-emerging though its prevalence in New Zealand is unknown.
Dietary sources of vitamin D are limited and the main source is skin synthesis on exposure to sunlight. The most recent
national survey indicated a high prevalence of vitamin D insufficiency in New Zealanders.16 Plasma concentration
of 25-hydroxyvitamin D is a marker of vitamin D status. A level below 25 nmol/L indicates risk of vitamin D deficiency.
A survey of pregnant women from a general practice population in Wellington reported that 87% of women had 25-hydroxyvitamin
D below 50 nmol/L.17
Many experts agree that the recommended adequate intake for vitamin D of 200 IU per day during pregnancy is grossly
underestimated.18 Studies are currently underway to address the effect of vitamin D supplementation during
pregnancy on the nutritional vitamin D status in both mother and foetus.
There is little evidence to support other supplements
For all other vitamin and minerals in pregnancy, there is little evidence to support routine supplementation unless
inadequate nutrient intakes are suspected.
Women who are taking multivitamin/multimineral supplements should be cautioned
to avoid exceeding intake of 10,000 IU (3,330 RE) of vitamin A (retinol) per day.
Get a pdf of the table here
References
- Schader I, Corwin P. How many pregnant women in Christchurch are using folic acid supplements in early pregnancy?
NZ Med J 1999;112:463-5.
- Dobson I, Devenish C, Skeaff CM, Green TJ. Periconceptional folic acid use among women giving birth at Queen Mary
Maternity Hospital in Dunedin. Aust NZ J Obstetrics and Gynaecology 2006;46:534-7.
- Hauger MS, Gibbons L, Vik T, Beliz�n JM. Prepregnancy weight status and the risk of adverse pregnancy outcome. Acta
Obstet Gynecol Scand. 2008;87(9):953-9.
- Ministry of Health. 2008. A Portrait of Health: Key results of the 2006/07 New Zealand Health Survey. Wellington:
Ministry of Health.
- Olsen CM. Achieving a healthy weight gain during pregnancy. Ann Rev Nutr. 2008;28:411-23.
- Institute of Medicine, Food and Nutrition Board, Committee on Nutritional Status During Pregnancy and Lactation,
Subcommittee on Dietary Intake and Nutrient Supplements During Pregnancy, Subcommittee on Nutritional Status and Weight
Gain During Pregnancy. Nutrition during pregnancy. Part I - Weight gain. Part II - Nutrient supplements. Washington,
DC: National Academy Press; 1990.
- Linne Y, Dye L, Barkeling B, Rossner S. Long-term weight development in women: A 15-year follow-up of the effects
of pregnancy. Obes Res. 2004:12:1166-78.
- Stotland NE, Haas JS, Brawarsky P, Jackson RA, Fuentes-Afflick E, Escobar GJ. Body mass index, provider advice, and
target gestational weight gain. Obstet Gynecol. 2005;105(3):633-8.
- Cogswell ME, Scanlon KS, Fein SB, Schieve LA. Medically advised, mother's personal target, and actual weight gain
during pregnancy. Obstet Gynecol. 1999;94:616-22.
- Beard JL, Hendricks MK, Perez EM et al. Maternal iron deficiency anemia affects postpartum emotions and cognition.
J Nutr 2005;135:267-72.
- Thomson CD, Packer MA, Butler JA, et al. Urinary selenium and iodine during pregnancy and lactation. J Trace Elem
Med Biol 2001;14:210-7.
- Zimmerman MB. The adverse effects of mild-to-moderate iodine deficiency during pregnancy and childhood:a review.
Thyroid. 2007;17:829-35.
- Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating
women and in children less than 2 years old: conclusion and recommendations of the technical consultation. Public Health
Nutr 2007;10(12A):1606-11
- Sullivan K. Iodine supplementation for pregnancy and lactation: United States and Canada: recommendations of the
American Thyroid Association. Thyroid 2007;483-4.
- Morley R, Carlin JB, Pasco JA, Wark JD. Maternal 25-hydroxyvitamin D and parathyroid hormone concentrations and offspring
birth size. J Clin Endocrinol Metab. 2006;91(3):906-12.
- Rockell JE, Skeaff CM, Williams SM, Green TJ. Serum 25-hydroxyvitamin D concentrations of New Zealanders aged 15
years and older. Osteoporos Int. 2006;17:1382-9.
- Judkins A, Eagleton C. Vitamin D deficiency in pregnant New Zealand women. NZ Med J. 2006;119
- Hollis BW. Vitamin D requirement during pregnancy and lactation. J Bone Miner Res. 2007;22 Suppl 2:V39-44
- Australian Government. Department of Health and Ageing. National Health and Medical Research Council. Ministry of
Health New Zealand. Nutrient reference values for Australia and New Zealand including recommended dietary intakes. 2006