View / Download pdf
version of this article
New Zealand has one of the highest rates of childhood asthma in the world with 25% of children aged six to seven years
and 30% of adolescents 13–14 years reporting asthma symptoms. The prevalence has fallen in the last decade, but
significant challenges remain. Among these are diagnosis, adherence and ethnic disparities in treatment.
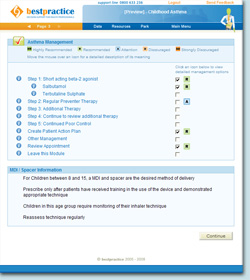
Bpac has recently published and circulated a guide to the management of
childhood asthma which is based on the New Zealand childhood asthma guidelines and other international sources. The
guide is designed to complement the bestpractice childhood asthma decision support tool.
Inequalities in asthma prevalence, morbidity and mortality
bestpractice Decision Support module
The module will assist the practitioner in the diagnosis, management and monitoring of asthma in children, including
the generation of an individual action plan.
This module is available free to general practice. For further information contact:
Jamie Murley
bestpractice Decision Support
Phone: 03 479 2816
Fax: 03 479 2569
Email: jamiem@bpac.org.nz
Key results of the 2006/07 New Zealand Health Survey, show that one in seven children aged 2–14 years (14.8%)
had been diagnosed with asthma and were taking medication for this condition. Adjusted for age, there were significantly
more Māori children taking medication for asthma than other children in the total population.
Prevalence rates for asthma are higher for Māori (26%) and Pacific children (22%) than for European/other children
(20%) and this disparity increases with age.
Māori and Pacific children with asthma suffer more severe symptoms than other children, are hospitalised more frequently,
and have more days off school as a result of their asthma.
The guide emphasises the ethnic disparities that exist in the prevalence, treatment and outcomes of childhood asthma
and suggests strategies to improve management in all groups.
Reliever to preventer ratio
Data shows that the ratio of reliever to preventer dispensings is higher in Māori and Pacific children than in European/other
children This means that Māori and Pacific children are more likely to depend on an asthma reliever (such as salbutamol)
and less likely to use inhaled corticosteroids than European/other children. Māori also appear to be less likely
to be prescribed a long acting beta-2 agonist. Both the guide and the bestpractice decision support module provide guidance
on diagnosis, medicines management and patient/carer information.