Troponins have overtaken the traditional ‘cardiac enzymes’, and can provide valuable information of the likelihood of a myocardial infarct. Although troponins are recognised as having diagnostic advantages over older cardiac enzymes, it is important the test is requested appropriately.
In this article 
View
/ Download pdf version of this article
Keypoints |
- Where clinical suspicion of MI is high (eg typical symptoms) refer immediately: do not test troponin
- Where clinical suspicion of MI is low (eg atypical symptoms or delayed presentation): troponin may be useful
- Negative troponin from the laboratory (measured at least 10 hours from onset of symptoms) can rule out almost all
myocardial events
- Positive troponin (from either a laboratory or point-of-care) is an indication for immediate referral
- Troponin has no role as a screening test for cardiovascular disease (CVD)
|
| When is troponin useful in primary care? |
Symptoms suggestive of MI
|

refer immediately to secondary care
|
| As a CVD screening test |
 |
| Delayed presentation (typical ‘Monday morning’ consult) |
 |
Atypical symptoms of MI
|
 |
| No ECG changes |
 |
|
Introduction
Troponins have overtaken the traditional ‘cardiac enzymes’, and can provide valuable information of the
likelihood of a myocardial infarct (MI). Although troponins are recognised as having diagnostic advantages over older
cardiac enzymes, it is important the test is requested appropriately. This is mainly because results are typically not
useful in the first one to three hours and maximum sensitivity is not until after 10 or more hours following onset of
acute MI.
Where clinical suspicion of MI is high (eg typical symptoms) refer immediately. Do not test troponins
There is almost no use for troponin in an acute presentation of possible MI in primary care. Measurements of troponin
are likely to remain normal immediately after an acute MI and it takes several hours before a useful result can be obtained.
Therefore, a single early negative test is not useful.
When a patient presents to primary care with acute chest pain suggestive of MI, the role of the GP is well defined.
Immediate transfer to hospital/cardiac care is indicated. This should not be delayed by waiting for the troponin result.
Where clinical suspicion of MI is low (eg atypical symptoms or delayed presentation) troponin is a useful test
There are a number of situations when the GP has a less clear pathway to follow, which may include situations such as
atypical symptoms, presentation several days after the onset of chest pain, or no ECG changes. For these situations, troponin
may be a useful test.
A common scenario in which troponins may be useful is for patients presenting 24-72 hours after a single episode of
chest pain, ‘the Monday morning consult’. Measurement of troponin and an ECG will establish whether or not
the chest pain was due to a MI. If there has been a MI, troponin is likely to remain elevated for up to 10 days. A positive
troponin result is indication for immediate referral.
It has been estimated that approximately 20% of all MIs are unrecognised with the patient presenting with symptoms which
are not initially suggestive of MI.1,2 Atypical presentations are more common in women, people with diabetes
and older people.3 Troponins are a useful rule-out test when there is a low clinical suspicion of MI, as long
as the poor sensitivity of early measurement (within the first 10 hours of the onset of symptoms) of troponin is recognised.
For patients presenting with symptoms that may be attributable to MI, but the ECG shows no ST elevation, troponin is
a useful discriminatory test and has been shown to increase the proportion of patients subsequently identified with MI,
and increase the accuracy of risk assessment.4
For patients with negative results initially, but for whom there is continuing suspicion, or there is the return of
possible ischaemic symptoms, repeat testing should be considered.
A laboratory measured negative test after 10 hours effectively rules out cardiac damage.
Other causes of raised troponin level
In the presence of typical symptoms and a high suspicion of an MI, a raised troponin level confirms the diagnosis of
cardiac ischaemia. However when the clinical picture is not typical, a raised troponin level is not diagnostic for ischaemic
damage.
On some occasions patients may have increased troponins as a result of a process other than myocardial ischaemia leading
to MI. These include severe heart failure, pulmonary embolism, myocarditis, pericarditis, cardiomyopathy, trauma and any
other cause of damage to cardiac muscle.
Troponin elevations are also common in people with end-stage renal disease (where cardiac death is common), but the
clinical interpretation of these results remains unclear. In patients with known renal disease who present with symptoms
of MI, a single high troponin result needs to be interpreted with caution as the result could either be due to acute MI
or underlying renal disease.5
Troponin has no role in ‘screening’ for CVD
Cardiologists in New Zealand have previously expressed concern6 at the increasing use in primary care of
troponin as a screening test. Some GPs are requesting troponin checks several weeks or even several months in advance. There
is no rationale for this and the practice is strongly discouraged.
Troponin has no role as a risk marker for CVD risk assessment in primary care and there is no indication for undertaking
troponin testing in asymptomatic patients. Troponin testing should be confined to symptomatic individuals only.
Laboratory versus point-of-care troponin testing
A negative troponin result is an appropriate ‘rule out’ test for MI, only if a laboratory method is used
and if the initial symptoms occurred more than 10 hours ago. Most point-of-care methods for troponin testing do not have
sufficient sensitivity to ‘rule out’ acute MI.
However, a positive result for troponin, whether from the laboratory or point of care, is significant, indicating myocardial
damage. In the presence of typical symptoms it is strongly predictive of MI even if there are no ECG changes.
What are troponins?
Troponin is a 3-unit complex of troponin I, T and C, (T for ‘tropomyosin binding’, I for ‘inhibitory’,
and C for ‘calcium binding’). These are located at regular intervals along the length of actin filaments
and play a key role in muscle contraction. Troponin I (TnI) and T (TnT) have cardiac specific isoforms and are used for
assessing cardiac injury.5 Apart from their proximity to each other in the troponin complex, troponin T, C
and I are otherwise unrelated proteins.
Troponin testing is widely available throughout New Zealand, but there is some variation as to whether TnI or TnT is
tested by individual laboratories. TnT and TnI are different tests and results cannot be used interchangeably. Different
laboratories use different assays for these tests and the results between laboratories cannot be compared.
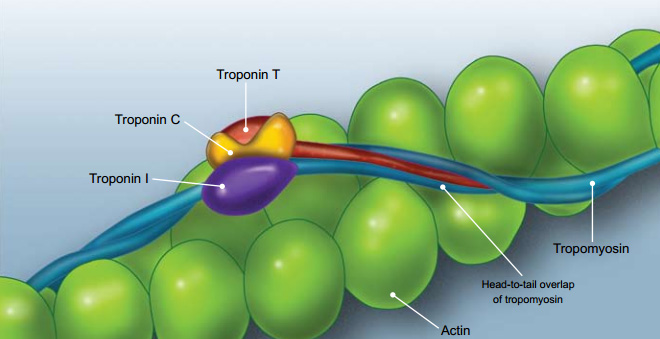
Figure 1: Troponin complex in cardiac muscle9 |
Troponins are now considered the biomarker of choice for detecting cardiac injury and have surpassed the historical ‘cardiac
enzymes’ creatine kinase (CK), aspartate transaminase (AST) and lactate dehydrogenase (LDH), which are not specific
to cardiac muscle. Testing for cardiac troponin is associated with fewer false positive and false negative results.
Serum troponin concentrations begin to rise 3-4 hours following acute MI, and remain elevated for 7-10 days for TnI
and 10-14 days for TnT.10 Results are typically not useful in the first one to three hours and maximum sensitivity
is not until after 10 or more hours following onset of acute ischaemia.
The initial increase is due to troponin release from the cytoplasm, followed by the slower release of troponin from
the cardiac myofilaments as they degrade. This pattern of release means that troponins can be detected in the serum for
an extended period of time. See Figure 2 for a comparison of troponin release with ‘traditional’ cardiac
enzyme release patterns.
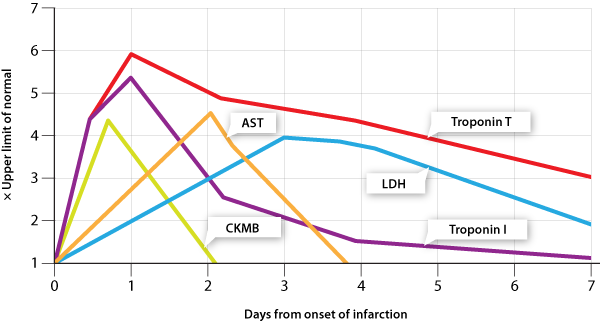
Figure 2: Temporal release patterns of troponins, CKMB, AST and LDH11,12
Acknowledgement
Thank you to Dr Michael Crooke, Chemical Pathologist, Wellington, for expert guidance in developing
this article.
References
- Kannel W, Abbott R. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study.
New England Journal of Medicine. 1984; 311:1144.
- Baker G, Koelmeyer T. Death due to unrecognised myocardial infarction causing left ventricular rupture: can we improve
the diagnostic rate? New Zealand Medical Journal. 19; 112:429-30.
- Guidelines for the management of acute coronary syndromes 2006. Acute Coronary Syndrome Guidelines Working Group.
Med J Aust. 2006 Apr 17;184(8 Suppl):S9-29.
- Cannon C, Turpie A. Unstable angina and non-ST-elevation myocardial infarction: initial antithrombotic therapy and
early invasive strategy. Circulation. 2003; 107:2640. Available from:
http://circ.ahajournals.org/cgi/reprint/107/21/2640
- Babuin L, Jaffe A. Troponin: the biomarker of choice for the detection of cardiac injury. Canadian Medical Association
Journal. 2005; 173:1191.
- BPAC. Laboratory Testing for Cardiovascular Risk. October 2007. Available from: www.bpac.org.nz
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin
assays. New Engl J Med 2009; 361: 858-867
- Keller T, Zeller T, Peetz D, et al. Sensitive troponin I assays in early diagnosis of acute myocardial infarction.
New Engl J Med 2009; 361: 868-877
- Chaikhouni A, Al-Zaim H. Troponin I Levels After Coronary Bypass Operations In Aleppo, Syria. Heart Views 2007;8(1):6-9
Available from:
http://www.hmc.org.qa/heartviews/VOL8NO1/02ORIGINAL_ARTICLE1.htm
- Morrow D, Cannon C, Jesse R, et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines:
Clinical Characteristics and Utilization of Biochemical Markers in Acute Coronary Syndromes. Circulation. 2007; 115:e356.
- Sanja Dacic, MD, PhD and Mohamed A Virji, MD, PhD Profiles of Total CK, CK-MB and Troponin I in Acute Myocardial
Infarction (AMI) Available from:
http://path.upmc.edu/cases/case178/dx.html
- University of Manchester, Department of Clinical Biochemistry. Supplementary biochemistry information for the problem
based learning cases. Markers of Myocardial damage