View / Download pdf
version of this report
Zopiclone, temazepam and triazolam for the treatment of insomnia
Zopiclone and some benzodiazepines, such as temazepam and triazolam, are indicated for the short-term treatment of insomnia.
Zopiclone is the most widely used hypnotic in New Zealand, with approximately 193, 001 patients dispensed this medicine
in 2014. It is used much more widely than benzodiazepines indicated for the treatment of insomnia, with approximately
25, 783 patients being dispensed temazepam in 2014, and 23, 556 dispensed triazolam. Zopiclone has been the 15th highest
prescribed medicine dispensed in the community in New Zealand for the last two years.1,2
Key messages:
- Due to adverse effects and the potential for dependence, zopiclone and benzodiazepines should not be used to treat
insomnia on a long-term basis
- Due to reduced renal clearance and an increased risk of falls, long-acting benzodiazepines and high doses of benzodiazepines
or zopiclone should be avoided in elderly patients
- Behavioural interventions have greater overall success rates than medicines for the treatment of insomnia in the long
term, and are safer3
- Engagement and regular discussion with nursing staff in aged care facilities can help reduce the number of elderly patients
taking medicines for insomnia in these facilities4
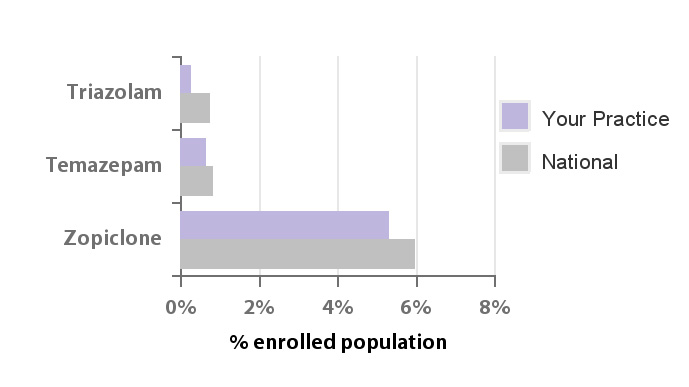
Hypnotic dispensing in your practice and New Zealand
Approximately 6.0% of the New Zealand population enrolled in primary care were dispensed zopiclone in 2014, and 0.7
– 0.8% of patients were dispensed temazepam or triazolam (Figure 1). Of patients using temazepam, triazolam
or zopiclone in 2014:
Figure 1. Hypnotic dispensing in your practice and New Zealand
Duration and volume of use suggests dependence is common
Nationally, 26% of all patients dispensed zopiclone, temazepam or triazolam in 2014 collected a prescription for at
least one of these medicines in each quarter of the year, suggesting long-term use by these patients.
Table 1 shows the number of patients registered to your practice who are likely to be long-term users.
They were dispensed at least 365 tablets of these medicines in 2014, some of which may have been prescribed by clinicians
outside of your practice.*
Table 1. Registered patients dispensed at least 365 tablets in 2014 for sample practice and New Zealand
| Zopiclone |
n |
% of all patients dispensed zopiclone |
| Sample Practice |
10 |
12% |
| National |
16,164 |
8% |
| Temazepam |
n |
% of all patients dispensed temazepam |
| Sample Practice |
1 |
25% |
| National |
2,980 |
12% |
| Triazolam |
n |
% of all patients dispensed triazolam |
| Sample Practice |
1 |
100% |
| National |
3,575 |
15% |
Use is high in older people - Nationally 35%
Adults aged 65 years and over make up approximately one-third of patients dispensed zopiclone, triazolam or temazepam.
Due to reduced renal clearance benzodiazepines and zopiclone can have a longer half life when taken by elderly people.
Since these medicines can affect balance and increase the risk of falls, consider whether the benefits outweigh the risks
of use in elderly patients; when prescribed, lower doses are recommended.
 of Sample Practice patients dispensed zopiclone, temazepam
of Sample Practice patients dispensed zopiclone, temazepam
or triazolam were aged 65 years or older.
Tips for your practice:
- If your practice has patients who are collecting prescriptions for hypnotics throughout the year, consider initiating
discussion about adverse effects and strategies for withdrawing. For further information on withdrawal, see:
www.bpac.org.nz/BPJ/2015/February/benzodiazepines.aspx
- Older patients using hypnotics may be at increased risk of fractures from falls; a focus on falls prevention
is beneficial in this patient group
- Other adverse effects of hypnotics may be experienced by patients of any age, and are associated with increasing cumulative
dose; prevent patients from becoming dependent on hypnotics, by prescribing short courses only and regularly
reviewing
* N.B. The numbers presented here include prescriptions from any practice or doctor; not just those prescribed
by your practice. Patients who are dependent on these medicines may see other doctors to increase the number of tablets
they are prescribed. Including only dispensings from your practice is likely to underestimate the true extent of zopiclone,
temazepam and triazolam use in patients under your care and therefore we have included dispensings from other doctors
and practices so you can more accurately gauge the number of patients under your care who may be using these medicines
inappropriately. An audit of your practice records may show a lower number of patients, and the difference is likely to
represent patients dispensed zopiclone, temazepam or triazolam where your practice was not the sole prescriber of these
medicines.
- Pharmaceutical Management Agency (PHARMAC). Annual review December 2014.
Wellington: PHARMAC, 2014. Available from:
www.pharmac.health.nz/about/annual-review/2014 (Accessed Apr, 2015).
- Pharmaceutical Management Agency (PHARMAC). Annual review December 2013.
Wellington: PHARMAC, 2013. Available from:
www.pharmac.health.nz/assets/annual-review-2013.pdf (Accessed Apr, 2015).
- Morin C, Benca R. Chronic insomnia. Lancet 2012;379:1129-41.
- Westbury J, Bindoff I, Peterson G. Expansion of the Reducing Use of Sedatives (RedUSe)
project to Australian Nursing Homes. Geriatric Psychiatry 2015;23:S155