In this article 
View / Download
pdf version of this article
Polypharmacy is a marker of potential problematic prescribing. In clinical practice, defining polypharmacy purely by a specific
number of medicines does not acknowledge that the potential risk of adverse effects of medicines can vary widely. However,
for the purposes of reporting on polypharmacy, it can be defined as the prescribing of five or more concurrent medicines,
and excessive polypharmacy as the prescribing of ten or more concurrent medicines. This report provides an update on
polypharmacy over a 12 month period (July 2013 – June 2014).
Key messages:1
- Not all polypharmacy is problematic - when the potential benefits outweigh the potential harms the use of multiple
medicines can be appropriate
- Older people are more likely than younger people to be affected by problematic prescribing and resulting medicine
adverse effects and interactions, due to multiple co-morbidities and reduced renal and hepatic function
- When deciding whether to add a medicine to a patients regimen, consider whether the symptom being treated is due to
an adverse medicine reaction (the “prescribing cascade”), what the goals of treatment are, what the expected
magnitude of benefit that the patient will receive from the treatment is and whether there are any non-pharmacological
treatments that can be considered instead
- An individualised assessment that includes a review of the need for each medicine can simplify treatment regimens
and reduce the potential for harm. “De-prescribing” may be the best clinical decision for some patients and
result in significant clinical benefits.
 Please see
BPJ 64 (October, 2014) for further information on polypharmacy
Please see
BPJ 64 (October, 2014) for further information on polypharmacy
Multiple Prescribers
It is increasingly recognised that health outcomes for patients are improved when one prescriber takes responsibility for all of
a patient’s medicines. An important reason for this is that as the number of prescribers increases, so too does the risk of problematic
prescribing and adverse medicine reactions.
Patients with polypharmacy are more likely to have multiple prescribers than those with few medicines.
Asking patients if they have visited another health professional is a simple way of checking if their medicine
regimen may have been altered.
Nationally between July, 2013 and June, 2014:
- Patients who received1 long-term medicine had an average of 2.5 prescribers
- Patients who received 5–9 long-term medicines had an average of 3.2 prescribers
- Patients who received 10+ long-term medicines had an average of 4.3 prescribers
National Trends
Over the last five years the proportion of the population experiencing either polypharmacy (five medicines) or excessive polypharmacy
(10+ medicines) has continued to increase with >11% of the population having five or more medicines between July 2013 and June 2014 (Figure 1).
These proportions have increased in all age groups over the last five years.
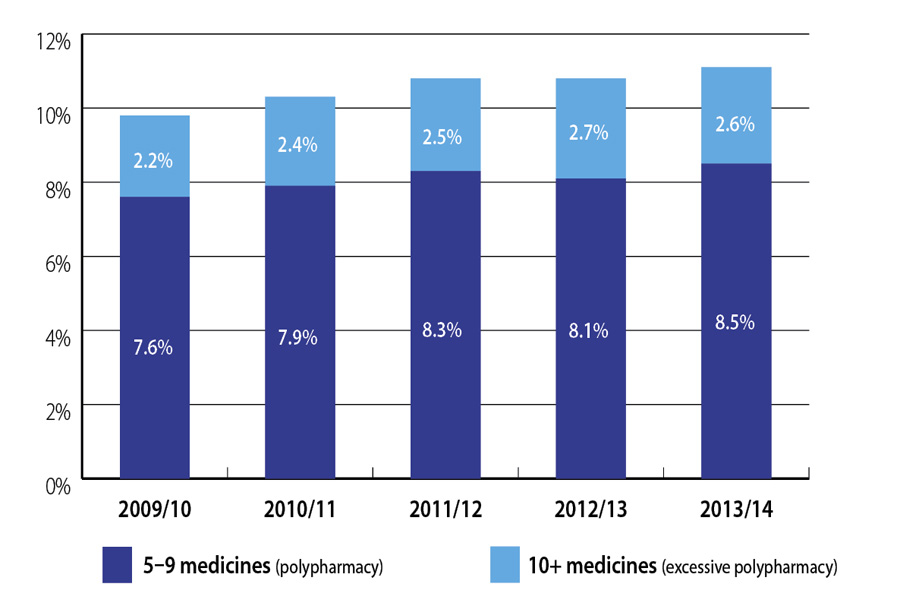
Figure 1. Proportion of polypharmacy in the New Zealand population over the last five years*
Sample Practice Data
While there are no criteria for optimal performance, this report is intended to help you benchmark your practice in
relation to national data on polypharmacy. It may highlight some target groups who could potentially benefit from a medicines
review or be used as a starting point for peer discussion around polypharmacy in your practice (Table 1).
Table 1. Proportion of registered patients with polypharmacy in New Zealand and your practice, July 2013–June 2014.*
|
NATIONAL DATA |
SAMPLE PRACTICE DATA |
| Age Band Years |
5–9 Medicines |
10+ Medicines |
Number of patients with 5-9 medicines |
Number of patients with 10+ medicines |
| 0–29 |
1% |
0% |
1% (22) |
0% (2) |
| 30–39 |
2% |
0% |
5% (33) |
1% (9) |
| 40–49 |
5% |
0% |
9% (77) |
2% (21) |
| 50–59 |
11% |
2% |
12% (103) |
3% (32) |
| 60–69 |
21% |
5% |
21% (142) |
9% (64) |
| 70–79 |
35% |
12% |
37% (136) |
19% (71) |
| 80+ |
42% |
23% |
38% (22) |
35% (83) |
Helpful tips for tackling polypharmacy2
- Always consider the option of discontinuing or reducing the dose of medicines
- Ensure you are comfortable that each medicine has a relevant indication
- Seek the advice of a pharmacist or clinical specialist if you are not sure whether a medicine is causing problems
or is able to be discontinued
- Agree on a course of action with the patient – they are more likely to follow a plan if they are part of the shared
decision-making process
*A medicine was counted as contributing to polypharmacy if the patient received three or more dispensing of that medicines in a year
- Best Practice Journal, Issue 64. (Accessed Oct,2014)
- Central Region District Health Boards. Available from
www.centraltas.co.nz (Accessed Oct, 2014)