Refer serious causes of red eye
"Stop!" Red flags
Patients with the following features should be referred urgently (same day) for ophthalmological assessment:1,
4
- Severe eye pain
- Severe photophobia
- Marked redness of one eye
- Reduced visual acuity (after correcting for refractive errors)
- Suspected penetrating eye injury
- Worsening redness and pain occurring within one to two weeks of an intraocular procedure
- Irritant conjunctivitis caused by an acid or alkali burn or other highly irritating substance, e.g. cement powder;
irrigate eye until pH neutral prior to referral (see below)
- Purulent conjunctivitis in a newborn infant (refer to a Paediatrician)
At this point in the consultation, the cause of the red eye may be obvious, e.g. foreign body, or the features may be
severe enough to warrant urgent referral. Table 1 summarises distinguishing features to determine the cause of a red eye.
Many patients with red eye may have ambiguous features and require a slit-lamp examination to be certain of a diagnosis.
If there is any suspicion of a serious cause then discussion with an Ophthalmologist is recommended. A triage assessment
by an Optometrist may also be useful, especially in remote locations.
Refer urgently for an ophthalmological assessment if the patient is suspected to have acute angle closure
glaucoma, iritis, scleritis, infectious/inflammatory keratitis or a penetrating eye injury.
Patients with a serious chemical eye injury also require urgent referral but the first priority is
irrigation of the ocular surface: topical anaesthetic should be applied, the eyelids held open and ≥ 500 mL of normal
saline or sterile water flushed across the globe, ideally using an intravenous giving set. Check the pH of the tear film
using litmus paper two to three minutes after each bag of fluid and repeat until the pH measures 7 – 8 and appears equal
between the two eyes.
Patients with an injury which has penetrated the eye should be referred immediately for an ophthalmological assessment.
Tetanus status should be determined, a hard shield taped over the eye (without exerting pressure on the globe), and the
patient instructed not to eat or drink in preparation for possible surgery. A penetrating injury may be obvious in the
case of a grossly misshapen globe or a full-thickness corneal or scleral laceration with prolapse of intraocular contents.
However, subtle clues to look for include a shallowing of the anterior chamber in that eye, or tear-drop distortion of
the pupil due to the iris prolapsing through an unnoticed wound, although these features may be difficult to detect without
the use of a slit lamp. Patients with an injury caused by a high-velocity object, e.g. when striking metal on metal, or
a sharp object, e.g. glass, thorn, knife, should be treated as having a high suspicion of penetrating injury, even if
no foreign object is visible.5
Management of acute angle closure glaucoma
This is a medical emergency and the patient should be discussed with an Ophthalmologist immediately to determine initial
management and arrange urgent assessment.
Symptoms of raised intraocular pressure are deep eye pain (described as throbbing, drilling pain), redness, blurred
vision (often with haloes around lights due to corneal oedema), headache, nausea and vomiting. Suggestive signs are ciliary
injection, fixed mid-dilated pupil, a generally hazy cornea and decreased visual acuity (Figure 3).
Although most General Practitioners will not have access to a tonometer (to measure the intraocular pressure), digitally
palpating the globe behind closed eyelids and comparing globe firmness provides useful information. In some circumstances
and locations an urgent intraocular pressure measurement by a local Optometrist may be indicated. While waiting, the patient
should lie flat with their face up, without a pillow. This may decrease the intraocular pressure by allowing the lens
and iris to "sink" posteriorly, opening up the drainage angle. The Ophthalmologist may recommend an immediate
dose of acetazolamide 500 mg, orally or IV, before a patient travels from a remote location.
Herpes simplex keratitis (dendritic ulcer)
Reactivation of the herpes simplex type 1 virus (“cold sores”) can, in some people, result in ocular symptoms; the
patient may not always be aware of a previous herpetic infection.
Active herpes simplex keratitis is an inflammation of the corneal epithelium due to viral replication and infection
causing characteristic dendritic corneal ulcers. Ulcers can be seen with fluorescein dye and appear as fine, branching
(i.e. dendritic) lesions (Figure 4).6 Without the use of a slit lamp, these lesions can easily be confused
with an abrasion (and vice versa).
Subsequent complications can include an inflammatory response (without active viral replication) inside the middle
layer of the cornea (stromal keratitis), or inside the eye (iritis/uveitis). There is usually no corneal epithelial defect,
therefore fluorescein staining is not seen in these conditions, although the cornea is usually hazy in stromal keratitis.6
Patients with suspected herpes simplex keratitis should be referred for ophthalmological assessment (or consider Optometrist
triage if uncertain and the use of a slit lamp would assist in diagnosis). Ocular anti-viral treatment is usually given
(aciclovir 3% eye ointment).6 Recurrences (almost always in the same eye) are common and can occur many years
after the previous episode. Long-term complications can include corneal scarring and visual loss.6
Management of keratitis, iritis and scleritis
Keratitis can result from several aetiologies, including bacterial keratitis (most commonly secondary to contact lens
use) or herpetic keratitis (see “Herpes simplex keratitis”). Key features are pain, photophobia
and decreased vision. In severe cases, a level of purulent exudate within the anterior chamber may be seen (a hypopyon).
Refer to an Ophthalmologist for treatment, which usually involves intensive topical antimicrobials.1
Iritis (anterior uveitis) is often very painful due to ciliary muscle spasm. Key features also include
photophobia and decreased vision, and the pupil will usually appear constricted with a poor light response and will sometimes
be distorted due to adhesions. Ophthalmological assessment will confirm the diagnosis and exclude any possible infectious
cause. Treatment (of non-infectious uveitis) involves topical, peri-ocular or systemic corticosteroids, as well as cycloplegics
(dilating drops) to reduce pain and prevent adhesions in the eye.
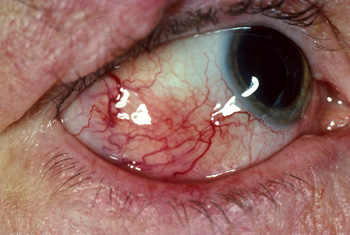
Scleritis (Figure 5) is characterised by severe, intense eye pain, described as deep, drilling pain,
like a toothache.1 It is usually associated with an underlying systemic autoimmune or inflammatory condition,
therefore treatment focuses on the systemic cause, after Ophthalmological assessment.
Endophthalmitis
Endophthalmitis is a sight- and globe-threatening internal infection of the eye. It is most commonly iatrogenic, occurring
after recent intraocular surgery (usually less than one to two weeks prior), but can rarely occur from endogenous causes
such as septicaemia or endocarditis. A patient may present with worsening pain, redness and/or visual loss. A level of
purulent exudate within the anterior chamber (a hypopyon) may be visible. Urgent ophthalmological assessment is required,
with treatment involving sampling of intraocular fluids, intravitreal antibiotics and possibly vitrectomy surgery.
 |
 |
Figure 5: Scleritis – showing localised conjunctival injection. Photo kindly supplied
by Dr Logan Mitchell, Department of Medicine, University of Otago. |
Figure 6: Viral conjunctivitis – showing diffuse conjunctival injection, watery discharge and
inflammation; typically presents sequentially in one eye, then the other eyes. Photo kindly supplied by Dr Logan
Mitchell, Department of Medicine, University of Otago. |
Managing red eye in primary care
Conjunctivitis
Conjunctivitis can be viral, bacterial or allergic. Bacterial and especially viral conjunctivitis are often highly contagious.
As a general rule, purulent discharge indicates bacterial conjunctivitis and a clear or mucous discharge indicates viral
or allergic conjunctivitis. The presence of pruritis, a history of atopy and exposure to a known allergen usually helps
to differentiate allergic conjunctivitis from viral.
Viral conjunctivitis is usually caused by an adenovirus. Typical features are sequential bilateral red eyes, watery
discharge and inflammation around the eye and eyelids, which can produce dramatic conjunctival swelling (chemosis) and
lid oedema, to the extent that the eye is swollen shut. The patient usually reports a feeling of grittiness or stabbing
pain, and may also have rhinorrhoea or other respiratory symptoms.10 Crusting of the lashes overnight can
sometimes be confused for a purulent discharge. Enlarged, tender preauricular lymph nodes are often present, and are a
useful feature to assist diagnosis.11
As there is no effective viricidal treatment against adenovirus, viral conjunctivitis is treated supportively. Advise
the patient to clean away secretions from eyelids and lashes with cotton wool soaked in water, wash their hands regularly,
especially after touching eye secretions, avoid sharing pillows and towels and avoid using contact lenses. Artificial
tear eye drops can be used if necessary to reduce discomfort.11, 12
Symptoms may take up to three weeks to resolve. In severe cases, punctate epithelial keratitis may develop – this can
be seen with fluorescein staining as multiple small erosions of the conjunctiva. Patients with this complication may report
ongoing discomfort for several weeks, which then resolves spontaneously.11 Immune sub-epithelial infiltrates
may develop after the conjunctivitis has settled, impairing visual acuity. These cannot be seen with fluorescein dye,
and can take several weeks to resolve spontaneously.
Bacterial conjunctivitis is usually caused by Streptococcus pneumoniae, Haemophilis influenzae, Staphylococcus aureus
or Moraxella catarrhalis. Less commonly, Chlamydia trachomatis or Neisseria gonorrhoeae may be the causative organism.
Symptoms are similar to viral conjunctivitis, but discharge is usually mucopurulent and may cause the eyelids to become
“glued” together after sleeping.11 Symptoms are usually more severe and persistent in patients with conjunctivitis
caused by Chlamydia trachomatis or Neisseria gonorrhoeae (termed hyperacute conjunctivitis).
Herpes zoster ophthalmicus (Shingles)
Herpes zoster ophthalmicus is essentially shingles (reactivation of the varicella-zoster virus) in the ophthalmic branch
of the trigeminal nerve (V).7 All parts of the eye innervated by this nerve can be affected, causing conjunctivitis,
keratitis and/or iritis, along with a periorbital vesicular rash, identical to a shingles rash seen elsewhere on the
body. Although a shingles rash that involves the tip of the nose (Hutchinson’s sign) is said to predict the development
of herpes zoster ophthalmicus, one-third of patients without the sign have ocular complications.7 Involvement
of other cranial nerves such as II (optic neuritis), III, IV and VI (diplopia) may suggest central nervous system involvement
and patients require neurological as well as ophthalmological assessment. Conjunctivitis and mild to moderate non-specific
keratitis are common acute presentations, with sight-threatening corneal stromal or intraocular inflammation more likely
to occur one to two weeks after the onset of vesicular rash.
Patients with suspected herpes zoster ophthalmicus should be started on oral acyclovir if they have presented within
72 hours of the onset of vesicular rash.7 Patients with decreased visual acuity and/or corneal epithelial
defect on fluorescein examination should be referred for same-day ophthalmological assessment.
Bacterial conjunctivitis is self-limiting in most people and symptoms resolve without treatment within
one to two weeks (although resolution may be more rapid in some people).11, 13 Advise supportive treatment
(as for viral conjunctivitis). Avoid the use of cosmetics applied to the eye area as these may be contaminated.
There has been much debate as to whether the use of topical antibiotics improves recovery time in people with bacterial
conjunctivitis. A 2012 Cochrane review of 11 randomised controlled trials concluded that the use of antibiotic eye drops
for bacterial conjunctivitis modestly improved the rate of “clinical and microbiological remission” and was associated
with a low risk of serious adverse effects.13 The meta-analysis found that after five days, symptoms had resolved
in 30% of patients receiving placebo and in 40% of those receiving a topical broad-spectrum antibiotic. By day ten there
was 41% remission in the placebo group and 50% remission in the antibiotic group.13
Most patients (or parents of young patients) who present to general practice with bacterial conjunctivitis will expect
to receive topical antibiotic treatment. The limitations of treatment should be explained and, if appropriate, offer a
“back pocket prescription” and instruct the patient (or parent) to delay starting treatment for a few days to see if the
symptoms resolve.11 Antibiotics may be started immediately if symptoms are severe or distressing. The recommended
treatment for adults and children aged over two years is chloramphenicol 0.5% eye drops, one to two drops, every two hours
for the first 24 hours, then every four hours, until 48 hours after symptoms have resolved. Chloramphenicol 1% eye ointment
can also be used at night in patients with severe infections or as an alternative to eye drops for those who prefer this
formulation. Fusidic acid 1% eye gel is an alternative to chloramphenicol, and is preferred in women who are pregnant;
one drop, twice daily, until 48 hours after symptoms have resolved.
 Pharmacists who have trained in the diagnosis and management of conjunctivitis
may sell chloramphenicol eye preparations, subject to conditions; appropriate verbal and written information on the self-management
of eye conditions must be given to all people purchasing these medicines.
Pharmacists who have trained in the diagnosis and management of conjunctivitis
may sell chloramphenicol eye preparations, subject to conditions; appropriate verbal and written information on the self-management
of eye conditions must be given to all people purchasing these medicines.
Laboratory investigations (i.e. a swab) to identify bacteria and sensitivity to antibiotics are not usually required,
but may be considered in immunocompromised patients or if symptoms are persistent despite chloramphenicol treatment.11 If
gonococcal conjunctivitis is suspected in an adult, collect an eye swab* (before applying any topical treatment) and test
for gonorrhoea and chlamydia.14
* This is normally the same type of swab as used for genital testing for chlamydia and gonorrhoea – check with your local laboratory
Dry-eye syndrome

Keratoconjunctivitis sicca, known as dry-eye syndrome, occurs when there is deficiency or dysfunction of the tear film
that normally keeps the eyes moist and lubricated.18 It is more common in females and incidence increases
with age.18 Decreased tear production is most often age-related, but can also be due to systemic auto-immune
diseases (e.g. Sjogren’s syndrome) or some medicines. Tear film dysfunction is often caused by blepharitis, altered lid
position (e.g. ectropion), decreased blink rate (e.g. intense concentration, Parkinson’s disease), incomplete lid closure,
or environmental factors.18
Symptoms include a feeling of dryness, grittiness or mild pain in both eyes, which worsens throughout the day. Eyes
water, especially when exposed to the wind.18 Patients are often aware that blinking or rubbing the eyes
relieves symptoms. Conjunctival injection is usually mild, and fluorescein staining typically shows punctate epithelial
erosions, which occur due to desiccation on the lower part of the cornea where lid coverage is least. The erosions are
very small and may not be seen without magnification.
Treatment includes eyelid hygiene the use of artificial tears and managing exacerbating factors, e.g. limiting use
of contact lenses, avoiding smoking, taking frequent breaks when concentrating on a screen.18 In some cases,
punctal plugs are inserted into the lower or upper tear drainage canals of the eye, to reduce dryness.
Complications of dry-eye syndrome include conjunctivitis and keratitis.
Newborn infants: If conjunctivitis is present in a newborn infant (aged ≤ 28 days), consider Chlamydia
trachomatis or Neisseria gonorrhoeae as the cause, usually transmitted vaginally during birth. Refer the infant urgently
to a Paediatrician; do not apply topical treatment. If the diagnosis is confirmed, parents will also require testing and
possible treatment. Gonorrhoea can result in a sight-threatening eye infection and chlamydia can be associated with the
development of pneumonia in young infants.11 N.B. Infants who present with a “sticky eye”, without conjunctival
inflammation, are most likely to have poor drainage of the lacrimal duct rather than conjunctivitis, and this does not
require urgent assessment.11
Allergic conjunctivitis is caused by a local response to an allergen, e.g. pollen, preservatives in
eye drops or contact lens solution. Patients typically present with swollen, itching eye(s), irritation, mild photophobia
and watery or serous discharge.1 Symptoms are episodic in the case of seasonal allergies. Eversion of the
lids often reveals a “cobble-stone” appearance of the tarsal (eyelid) conjunctiva because of the development of large
papillae or swellings of the subepithelial stroma (connective tissue).
Treatment is supportive; avoid the allergen where possible, avoid rubbing the eyes, apply a cool or warm compress to
relieve symptoms, use artificial tear eye drops if required. If symptoms are severe or other treatments are ineffective,
prescribe antihistamine eye drops, e.g. levocabastine, or a mast cell stabiliser (takes several weeks for full effect),
e.g. lodoxamide or cromoglicate sodium. Olopatadine eye drops combine antihistamine and mast cell stabilisation activity
and are often effective. An oral antihistamine may also be prescribed, depending on patient preference and previous response
to treatment.1
Patients with severe allergic conjunctivitis should have their visual acuity checked and a fluorescein examination,
and then be referred to an Ophthalmologist for further assessment and possible initiation of topical corticosteroids.
Vernal and atopic keratoconjunctivitis are two severe forms of allergic eye disease affecting children and young adults
respectively, and can be associated with large epithelial defects on the cornea (shield ulcers) that can lead to scarring,
and also microbial keratitis – especially if topical immunosuppressants are being used.
Foreign bodies and corneal abrasions
Patients with a foreign body in their eye or a corneal abrasion typically present with discomfort, watery discharge,
pain associated with movement of the eye, blurring of vision and photophobia.5
The patient may be aware of the foreign body which has entered the eye or it may have occurred unnoticed during an activity
such as chiselling, hammering, grinding metal or mowing the lawn. Corneal abrasion can occur due to an accidental scratch,
e.g. with a fingernail or while removing or inserting contact lenses, or by rubbing the eye, e.g. in the presence of a
foreign body.
Any patient with a penetrating eye injury (or suspected) should be referred immediately for ophthalmological assessment.
If ocular penetration is not suspected, examine the eye to locate the foreign body, which may be on the conjunctiva or
under the eyelid. N.B. Do not attempt to evert the eyelid if there is a possibility of a penetrating eye injury as the
contents of the eye may prolapse.5
Fluorescein dye can be used to help to detect the object or an abrasion. Although patients with a penetrating injury
should be referred for treatment, if the injury is missed, and the eye is stained, a penetrating injury will be seen as
a dark stream (i.e. dye diluted by aqueous) in a pool of bright green (i.e. concentrated dye); this is known as the Siedel
sign, although it may be difficult to see without a slit lamp.16
To remove a foreign object from the eye, first apply a topical anaesthetic, e.g. tetracaine. Oral pain
relief with paracetamol or ibuprofen can also be given.16 Depending on the nature and location of the foreign
object, it may be able to be removed by irrigating the eye. If this is not adequate, use a sterile cotton-tipped swab.
In some cases, a more precise tool, such as the bevelled edge of a sterile needle may be required.5 This should
always be held tangential (on an angle) to the surface of the globe, with the bevel facing the globe, to minimise the
chance of corneal perforation. This method can be difficult without the magnification provided by a slit-lamp microscope
– if unsure, arrange for the patient to be treated where a slit-lamp is available (Optometrist, hospital emergency department
or Ophthalmologist).
If the object is embedded and cannot be removed, or if after the object is removed there is a large abrasion, corneal
opacity, rust ring (after removing a metal object), a distorted pupil or reduced visual acuity, refer for ophthalmological
assessment.5
To prevent a secondary infection, in a patient with a corneal abrasion (including after removal of
a foreign object) prescribe chloramphenicol 0.5% eye drops, one drop, four times daily, for seven days (or ointment, depending
on patient preference). Fusidic acid eye gel 1%, one drop, twice daily, for seven days is an alternative.5
An eye patch or dressing is not necessary.12 Contact lenses should be avoided until the abrasion has healed
and ideally, until antibiotic treatment has finished. There is usually no need for prescription of anaesthetic drops;
prolonged use can lead to corneal damage.15
Ideally, the patient should be reassessed in 24 – 48 hours. Refer for an ophthalmological assessment (or consider Optometrist
triage) if the abrasion is not resolving, or if visual acuity deteriorates or pain increases.5
Subconjunctival haemorrhage
Subconjunctival haemorrhage occurs when blood vessels in the space between the sclera and the conjunctiva rupture. This
may be caused by blunt trauma to the eye, coughing, sneezing or straining. In some cases, it may be associated with atherosclerosis,
bleeding disorders or hypertension.12 Subconjunctival haemorrhage, while often dramatic in appearance, is
usually harmless. It is not associated with any significant pain and does not affect vision – if the patient has significant
pain, photophobia and reduced vision, reconsider the diagnosis and refer them for an ophthalmological assessment if uncertain.12
In most patients, subconjunctival haemorrhage will resolve without treatment in one to two weeks.12 Use
of artificial tears may relieve any discomfort. Check the patient’s blood pressure and, if they are taking warfarin, it
is recommended that their INR level is checked.12
Episcleritis
Episcleritis is a local inflammation of the superficial top layer of the sclera.12 Patients present with
dilated superficial blood vessels in a localised area of the sclera, as opposed to conjunctivitis which appears more diffuse.
Patients usually report mild pain only, discharge and photophobia are usually absent and vision is unaffected.12 Localised
tenderness is a helpful diagnostic feature.
Episcleritis resolves without treatment, within approximately three weeks. Artificial tears may be used to relieve discomfort,12 and
an oral non-steroidal anti-inflammatory drug (NSAID) such as ibuprofen, used if required. If symptoms worsen, consider
the possibility of scleritis.
Blepharitis
Blepharitis is a chronic inflammation of the margin of the eyelids, which can present in patients as a “red eye”, with
burning, pruritis and discharge. It is frequently seen in older people, and people with rosacea and seborrhoeic dermatitis.17 Blepharitis
is caused by dysfunctional secretions of the Meibomian glands, oil-secreting glands in the eyelid margin which help the
tears to distribute evenly across the ocular surface and decrease tear evaporation. These dysfunctional secretions lead
to a chronic inflammatory state within the lid, and the resultant dysfunctional tear film leads to dry eye symptoms and
signs (see “Dry-eye syndrome”). When diagnosing blepharitis, consider the possibility of squamous cell, basal cell or
sebaceous cell carcinoma of the eyelid margin (marked eyelid asymmetry may indicate this), dermatitis or infection (e.g.
impetigo).17
Treatment focuses on improving the Meibomian gland secretions, but is never curative and it should be explained to patients
that management needs to be ongoing. As blepharitis is a chronic condition, relapses and exacerbations can be expected.17
The following regimen should be initially carried out twice daily, then as symptoms improve, once daily:17
- Apply a warm compress to the closed eyelids for five to ten minutes
- Gently massage the eyelid margin with a circular motion
- Clean the eyelid with a wet cloth or cotton bud and rub along the lid margins; use a solution of 1 part baby shampoo
to 10 parts water for cleaning
The use of cosmetics around the eye should be avoided, especially eye liner. Artificial tears may assist in relieving
symptoms.
If the symptoms are particularly severe, topical antibiotics can be considered; chloramphenicol 0.5% eye drops, one
to two drops, four times daily, for seven days (or up to six weeks in chronic cases).12, 17 Fusidic acid eye
gel 1% is an alternative. In some cases, oral tetracyclines, e.g. low dose doxycycline, may be considered if topical antibiotics
have not resulted in an adequate response. Antibiotics are usually prescribed initially for six weeks, but may need to
be continued for up to three months, and repeated intermittently.17 Eyelid hygiene should be maintained throughout
treatment.
Blepharitis does not permanently affect vision, as long as complications are adequately managed.17 People
with blepharitis have an increased risk of developing conjunctivitis and keratitis.17 Long-term complications
include loss of eyelashes (madarosis), misdirection of lashes towards the eye (trichiasis) and depigmentation of the lashes
(poliosis).17